Migraines are not simply headaches. For millions of people, they are a complex neurological condition rooted in genetics, energy metabolism, inflammation, and hormonal fluctuations. Although symptoms may appear suddenly, the biological processes behind migraine development begin long before the pain starts. Modern research—from genetics to neuroimaging—now gives us a clearer picture of what actually happens inside the brain.
Genetic Predisposition: A Brain Born More Sensitive
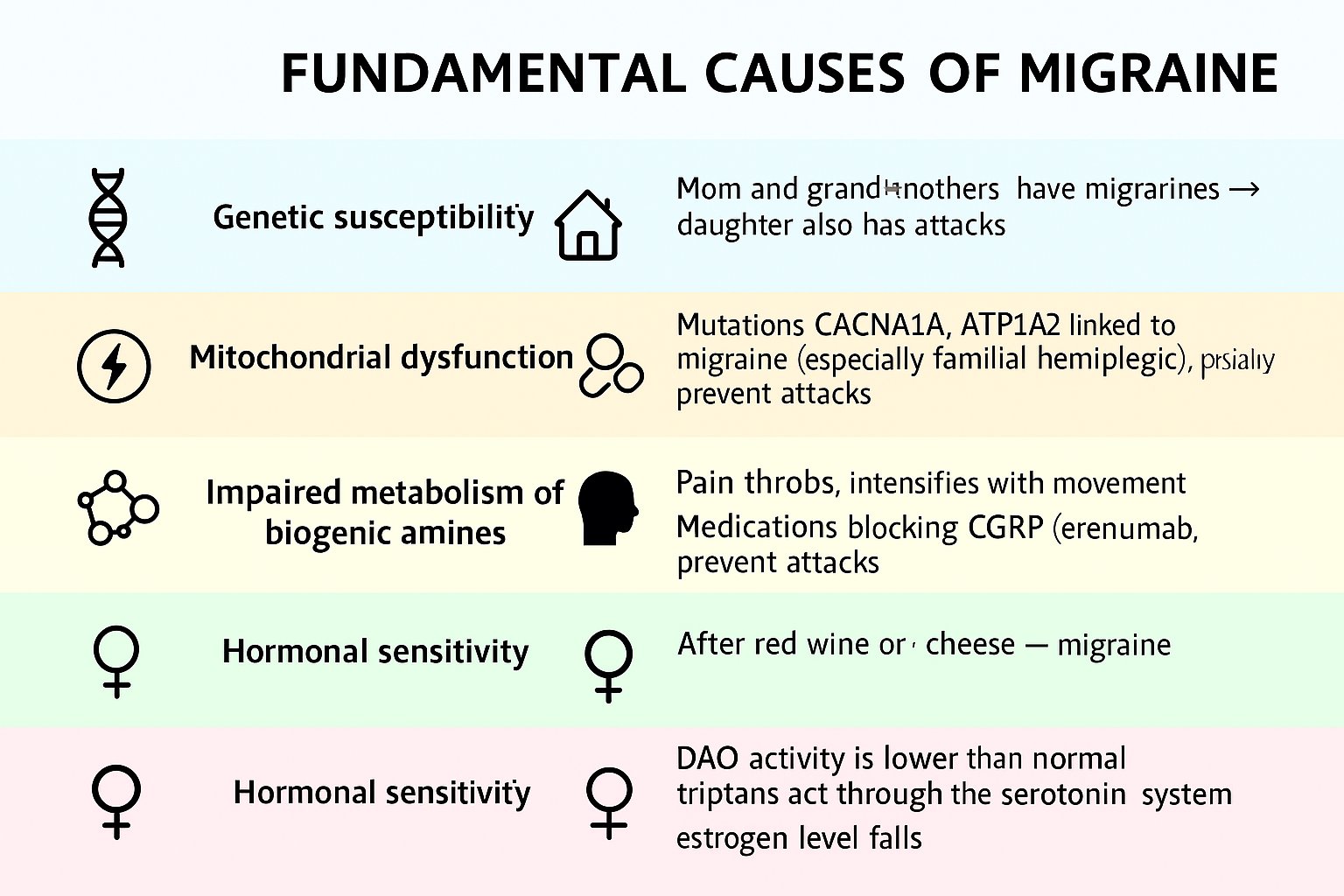
One of the strongest predictors of migraine is family history. If a mother or father experiences migraines, the likelihood that their child will also develop them increases dramatically. Scientists discovered that certain inherited variations in ion channel genes make neurons fire more easily than normal. In other words, the brain becomes hypersensitive.
This doesn’t mean a person is “weak” or “stressed.” It means their nervous system is biologically wired to react more intensely to triggers such as bright light, changes in sleep, dehydration, or hormonal shifts.
In rare genetic forms like familial hemiplegic migraine, mutations in CACNA1A, ATP1A2, and SCN1A show how deeply the roots of migraine extend into cellular function.
The implication is profound: migraines are not imagined or exaggerated—they are encoded at the microscopic level of neuronal signaling.
Mitochondrial Dysfunction: When the Brain Runs Out of Energy
A migraine-prone brain often struggles with energy production. Neurons require large amounts of ATP to function, communicate, and maintain stability. When energy drops—after poor sleep, skipping meals, or experiencing stress—the brain becomes vulnerable.
Imagine your brain as a city experiencing a temporary power shortage. Traffic lights flicker, systems slow down, and instability spreads. The same destabilization happens in the cortex, making a migraine more likely.
This is why supplements that support mitochondrial energy, such as riboflavin (B2), CoQ10, and magnesium, consistently show benefits in clinical studies. They don’t “cure” migraines, but they strengthen the brain’s ability to stay stable under pressure.
Neuroinflammation and the CGRP System
One of the biggest breakthroughs in migraine science is the discovery of the CGRP pathway. CGRP (calcitonin gene-related peptide) is a neuropeptide released by the trigeminal nerve during an attack. It dilates blood vessels, increases inflammation, and amplifies pain signals.
The pulsating, movement-sensitive pain that many people describe is not random—it is the direct effect of CGRP flooding the system.
The development of anti-CGRP treatments (like erenumab or fremanezumab) revolutionized migraine care because they target this exact mechanism. These medications block the receptor or the peptide itself, preventing the cascade that leads to inflammation and severe pain.
This discovery confirmed something patients have felt for decades: migraine pain is deeply biological, not psychological.
Scientific reference:
Independent clinical research published by the National Institutes of Health provides a detailed overview of how CGRP drives migraine inflammation and pain signaling.
Source: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6615327/
Biogenic Amine Metabolism Disorders: Histamine and Serotonin Imbalance
Many migraine attacks are triggered by foods like aged cheese, red wine, smoked meats, or chocolate. This is not a coincidence. These foods contain biogenic amines—compounds like histamine and tyramine—that must be broken down by enzymes such as DAO.
In some individuals, these enzymes work less effectively. As a result, histamine accumulates, serotonin balance is disrupted, and a migraine can begin.
Serotonin-based medications (like triptans or SSRIs) also interact with these pathways, which is why they provide relief for some patients and worsen symptoms in others.
This biochemical sensitivity explains why diet plays such an important role in migraine management—not as a “cure,” but as a way to stabilize vulnerable pathways.
Hormonal Sensitivity: The Hidden Influence of Estrogen
For many women, migraines intensify around the menstrual cycle. The reason is simple: estrogen levels drop sharply right before menstruation, and this fluctuation destabilizes the pain centers of the brain.
In fact, menstrual migraine is officially recognized in the International Classification of Headache Disorders (ICHD-3). It’s not a coincidence, not a mood change, not stress—it’s a physiological reaction to hormonal variation.
This hormonal sensitivity is also why migraines often improve during pregnancy (when estrogen is stable) and worsen during perimenopause (when estrogen fluctuates unpredictably).
Conclusion
Understanding the fundamental causes of migraine helps shift the perspective from “random pain attacks” to a clearly defined neurological condition with identifiable biological roots. Genetics, hormonal fluctuations, mitochondrial energy deficits, inflammation, and neurotransmitter imbalance all contribute to a brain that is exceptionally sensitive to internal and external triggers.
While no single factor explains every migraine, the combination of these mechanisms offers a powerful framework for prevention, treatment, and long-term management. The more awareness patients have about what is happening inside their brain, the more control they gain over their condition — and the less unpredictable migraines become.
Looking for personalized guidance?
Many migraine patterns become clearer when symptoms, triggers, sleep, nutrition, and medications are tracked consistently over time. Hope & Mo: Migraine and Medication Tracker helps uncover these hidden connections through AI-powered analysis, daily symptom logging, and treatment tracking.
👉 Learn more here: Hope & Mo: Migraine and Medication Tracker